Health
Dr Anshumalaa Shukla-Kulkarni, Consultant – Gynaecology, Laparoscopic and Robotic Surgery, Kokilaben Dhirubhai Ambani Hospital, sheds light on hysterectomy and when it may be required
Hysterectomy is the most commonly practised surgery in gynaecology, performed to remove the uterus with cervix, with or without tubes and ovaries. It is important to understand why the surgery is needed when the uterus is not functioning and be aware of the warning signs.
Menopause is the cessation of a woman’s menstrual cycle for more than a year owing to the non-functioning of ovaries. It means the ovaries stop producing oestrogen and progesterone and the monthly cycle stops. The normal age for menopause ranges from 45 to 55 years. If one continues to have periods after the age of 56, it is advisable to undergo a hysterectomy as prolonged exposure to oestrogens can cause cancers.
If you are over the age of 60, you need to watch out for the red flags. If you experience any of the following warning signs, get your body checked immediately by a gynaecologist.
- POST-MENOPAUSAL VAGINAL BLEEDING: This is by far the most important symptom to report to your gynaecologist. When you have attained menopause, the ovaries and uterus cease to function and there is no bleeding. Hence any bleeding—spotting or heavy—needs a check-up. The reasons could range from a treatable infection causing bleeding to overgrowth of the uterus lining, which may lead to cancer. After examination by a gynaecologist, you may need to undergo an ultrasonography of the uterus to check the lining and that of the ovaries. The acceptable limit of lining is 5 mm; anything more than that will need a small procedure called a hysteroscopy and endometrial biopsy. If you haven’t had a pap smear done for cervical health, please ask for one.
- THICKENED ENDOMETRIUM: This condition could be owing to endometrial hyperplasia. Hyperplasia is excessive growth of the lining which may be premalignant; this will be confirmed with a biopsy. Then, depending on the grade of severity, you may be advised surveillance (ultrasonography every year) or a hysterectomy.
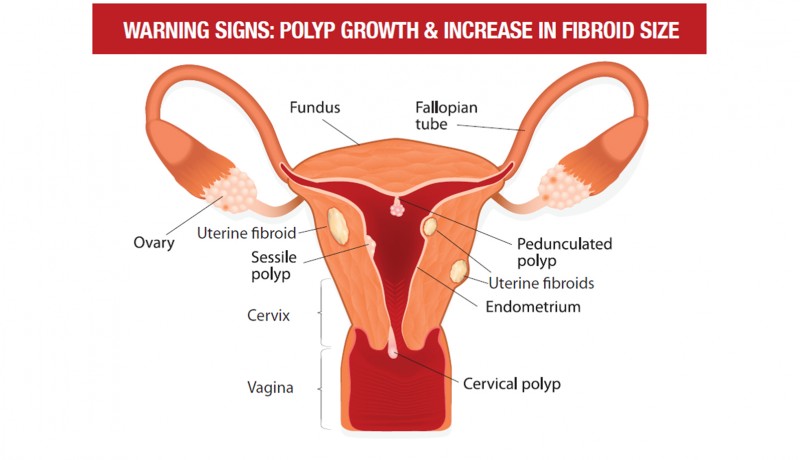
- POLYP GROWTH: Occasionally, post-menopausal bleeding may be a result of normal polyps (growth on the inside of uterus). This usually exists from the menstrual phase but gets detected after an episode of bleeding and also requires a hysteroscopy. The procedure is very simple; under anaesthesia, we introduce a 3-mm telescope to visualise the internal cavity of the uterus to identify the polyp and use scissors to cut it out.
- PROLAPSE: If you experience dysuria (painful or difficult urination), increased frequency of urination, burning micturition (urination) and difficulty in passing stools, or feel as if something is hanging down your vagina causing discomfort in walking, consult your doctor immediately. This could be owing to a prolapse or shift in the position of the uterus, bladder or rectum. The muscles that support the organs in your pelvis (uterus, bladder and rectum) are like a plate that runs from your backbone (sacrum) to the front bone (pubis) and is attached at the sides. With increasing age, this loosens and tends to hang down and causes the organs to shift. If the uterus remains out for longer periods of time, it causes difficulty in walking and, at times, cessation of urination. It may be just the urinary bladder or rectum hanging down that causes difficulty in passing urine or stools. In the initial stages, this condition can be treated with pelvic floor exercises; however, the second grade of prolapse or later requires surgical correction. At such times, it is advisable to remove the uterus and repair the defects, as it is easier to support organs without the weight of the uterus. This is done either through the vaginal route or a minimal access route (robot-assisted laparoscopy).
- PERSISTENT OVARIAN CYSTS: As menopause implies the cessation of ovarian function, any mass or cyst that grows in the ovaries after menopause needs to be checked and removed at the earliest. The chances of ovarian malignancy rise after 60; hence, anyone with a family history of cancer should get ultrasonography regularly. Routine check-up of the ovaries helps to detect ovarian cancerous or noncancerous cysts earlier. Ovarian cancer does not have specific symptoms; it is usually detected at an advanced stage.
- INCREASE IN FIBROID SIZE: Fibroids are excessive growth of the uterine muscles and can be very troublesome during periods. After menopause, they generally shrink and do not cause any issues. However, if there is a sudden increase in the size of fibroids or you notice a new fibroid growth, it needs urgent removal. The incidence of cancer of the fibroids is low but in these cases an early surgery could be life-saving.
- RECURRENT VAGINAL DISCHARGE: If you experience a recurrent foul-smelling vaginal discharge, visit the doctor immediately. Regular pap smears are highly recommended till the age of 65. As the incidence of cervical cancer is high after the age of 75, regular examinations are recommended.
- HISTORY OF CARCINOMA: A family history of carcinoma of the breast, ovary, endometrium and colon with a gene-dependent cancer may also require hysterectomy with bilateral salpingo-oophorectomy (surgery to remove the ovaries and fallopian tubes).
THE PROCEDURE
Hysterectomy can be done as an abdominal (through a large cut on the abdomen), vaginal (through the vagina), laparoscopic or robot-assisted (keyhole surgery) procedure. Total laparoscopic hysterectomy and robot-assisted hysterectomy are the best options for prolapse and cancer cases. This involves only three 5-mm cuts on the abdomen, through which the surgery is completed. There is decreased intra-operative blood loss, morbidity and postoperative pain, less analgesia is required, recovery is faster and stay in the hospital is shorter. In fact, patients get discharged within 48 hours of surgery.
AFTER-EFFECTS OF HYSTERECTOMY
Perimenopausal women may experience certain changes owing to the low oestrogen levels in the body. This is most commonly seen when both ovaries are removed.
- Ninety per cent of surgically induced menopausal women experience frequent and severe hot flashes compared to the 40 per cent of women who undergo natural menopause
- Night sweats
- Breast and vaginal atrophy
- Urogenital changes (recurrent urinary tract infection)
- Sexual dysfunction and decreased libido
- Shrinking of vaginal canal in length and diameter
- Increase in the pH balance of the vagina (allowing more pathogenic bacterial colonisation)
- Decrease in vaginal lubrication
- Thinning of vaginal mucosa and loss of elasticity
- Reduction in the distance from the urethral opening to vaginal introitus (opening that leads into the vaginal canal) owing to tissue atrophy
- Cardiovascular diseases like heart attack
- Stroke
- Osteoporosis
- Depression
The above-mentioned changes are not prominent in postmenopausal hysterectomy as the ovaries are non-functional. The dominant hormone in menopause is androstenedione (male hormone) that helps to keep the bones healthy. Hence, supplements are advised to the patient after a hysterectomy to maintain good physical and mental health.
THE WAY FORWARD
Non-hormonal treatments such as dietary modification, lubricants, phytoestrogens (plant estrogens found in soya), calcium and Vitamin D supplements help combat the symptoms. Hormone replacement therapy (HRT), where synthetic hormones available in the form of oral tablets, local vaginal oestrogen creams or patches (in case of severe symptoms), is also advised. Note: In patients with osteoporosis, HRT should be taken only under a doctor’s supervision.
Featured in Harmony — Celebrate Age Magazine March 2018
you may also like to read
-
Hot tea!
If you enjoy sipping on that steaming hot cup of tea, think twice. New research establishes a link between drinking….
-
Weight and watch
If you have stayed away from lifting weights at the gym, thinking it might not be a good idea for….
-
Toothy truth
Research has established a clear association between cognitive function and tooth loss when cognitive function score was categorised into quintiles…..
-
PRODUCT OF THE MONTH
Automatic Blood Pressure Monitor Measure your blood pressure and pulse rate with no fuss Hypertension, or high blood pressure, could….