Health

Robotic-assisted gait training is helping patients with neurological disorders walk again, says Dr Abhishek Srivastava, Director, Centre for Rehabilitation, Kokilaben Dhirubhai Ambani Hospital, Mumbai
Walking is one of the most significant functions of the human body and difficulty in walking is one of the most important manifestations of ageing. Elderly people are prone to many neurological conditions such as stroke, Parkinson’s disease, peripheral neuropathy and falls, causing brain or spinal cord injury. These diseases and injuries can cause paralysis with inability to move the lower limbs and subsequent difficulty in walking. This inability to walk can have serious consequences including deconditioning syndrome, pressure sores, contractures, osteoporosis and increased risk of fractures.
To regain the ability to walk after a stroke is one of the main endeavours of neurological rehabilitation. This is often the deciding factor in whether a patient leads an active life or is homebound, in some cases relying on assistance from another person. Interestingly, our nervous system has the potential to change its structure and function, an ability known as neuroplasticity. Repetitive exercises encourage such structural and functional changes in the nervous system, which greatly improve the patient’s ability to handle the tasks presented. As a result, modern neurophysiological concepts of walking now focus on repetitive, task-specific exercises.
Training with a robotic treadmill
‘If you want to learn to walk, you have to walk’. Training with a robotic treadmill system such as LokomatTM is based on this concept and enables repetitive training in complex walking cycles to take place as early as possible. It consists of a robotic gait orthosis, overhead body weight offloading system and a treadmill. Patients are first made to walk in the air, called ‘nice walking’, to evaluate whether they can sustain
the continuous movements of lower limbs. The next stage is called ‘safe walking’, where they take steps on the treadmill with the help of the robotic orthosis. The duration of an average session is up to 30 minutes and a person can walk up to 1 km during this time. This is equivalent to about 1,300 steps whereas in a conventional physical therapy session of the same duration, a person can only walk up to 50 steps. This increased load of task-specific training unmasks the reorganisation of the neural circuits and leads to improved neurological/motor recovery.
Beyond the known positive effects of treadmill therapy with partial body weight support such as improved balance, better motor control of the lower extremities, faster walking and greater endurance, LokomatTM training is especially beneficial to stroke survivors with hemiparesis (weakening of an entire side of the body) in the area of an essential unchangeable component of movement: standing on one leg. This can also be used to initiate walking in persons with severe traumatic brain injury and in managing gait problems in multiple sclerosis, severe peripheral neuropathy, Parkinson’s disease or any other neurological illness.
It is also useful for patients with incomplete spinal cord injury, or in other words, for patients who still have some residual function in their arms and legs. While LokomatTM training does not cause any functional development in cases of complete paraplegia, it can lead to an improvement in secondary effects, such as stimulating the metabolism, stabilising circulation, reducing spasticity and long-term improvement of bowel and bladder function.
Is it passive walking?
Some people feel this training is passive walking. However, that’s not the case—multiple parameters can be altered during training. As patients regain new motor power, robotic assistance or guidance force is reduced, body weight support is reduced and the treadmill speed is gradually increased. The biofeedback mode allows patients to have a visual representation of the new movements regained in lower limbs on the computer screen in front of them. What’s more, the augmented feedback mode allows the patient to play a game on the computer screen, challenging both cognitive and motor abilities.
With the course of treatment, when patients gain enough motor power and control that they can do ‘overground’ walking with supervision or assistive gait aid, robotic-assisted training is stopped. However, patients with severe osteoporosis at the hips, contractures in lower limbs, morbid obesity, large open wounds on the trunk and lower limbs and unstable medical and neurological status are not fit for this type of training.
Clinical trials
In the past years, there were doubts over whether robotic-assisted gait training in combination with conventional therapy had advantages over conventional therapy alone. This remained up for debate until recently, as a number of randomised controlled trials often showed different results depending on patient population and study design. However, in 2014, a new Cochrane review (a meta-analysis where the highest level of clinical evidence can be reached) analysed 23 randomised controlled trials involving 999 stroke patients comparing normal care versus electromechanical and robotic-assisted gait training. The trial found evidence that robotic gait training actually had a significant effect on a patient’s walking ability. The results showed that stroke patients who received robot-assisted gait training in combination with physiotherapy were more likely to achieve independent walking than patients who received only conventional gait training. This effect was most obvious in patients treated early after injury (within the first three months) as well as in patients who were not able to walk at the beginning of their therapy. Nonambulatory patients also significantly increased their walking velocity in response to electromechanically assisted gait training. The results show that every fifth dependency in walking ability after stroke might be avoidable if electromechanical-assisted devices are used.
The progress card
In our experience over the past two years with more than 200 patients of stroke, traumatic brain injury, spinal cord injury, hypoxic encephalopathy and Parkinson’s disease, we have found significant improvement in lower limb motor power and functional recovery in achieving independent or supervised mobility. The improvement was maximum in patients who were started on robotic training in the early phase after the neurological insult, especially in the first few weeks after stroke or brain injury.
Achieving independent mobility is the most important goal. But the beauty is that even patients with neurological illness who can’t move one or both lower limbs and even upper limbs can be made to walk on the robotic gait trainer. This boosts morale and leads to significantly improved participation in the overall neurorehabilitation programme. In fact, most of our stroke or brain injury patients who were started on a comprehensive neurorehabilitation programme, including robotic training, achieved independent mobility in three months after the neurological insult.
In conclusion
Robotic-assisted training has significantly changed the management of patients with neurological illness and injuries. Many more patients are going home walking from the hospital, able to live independently, and going back to work. This further reduces the overall cost of care and the financial burden on the family and society.
Photo: Haresh Patel Featured in Harmony — Celebrate Age Magazine August 2017
you may also like to read
-
Hot tea!
If you enjoy sipping on that steaming hot cup of tea, think twice. New research establishes a link between drinking….
-
Weight and watch
If you have stayed away from lifting weights at the gym, thinking it might not be a good idea for….
-
Toothy truth
Research has established a clear association between cognitive function and tooth loss when cognitive function score was categorised into quintiles…..
-
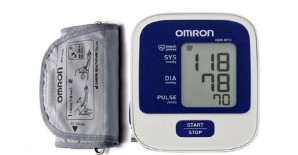
PRODUCT OF THE MONTH
Automatic Blood Pressure Monitor Measure your blood pressure and pulse rate with no fuss Hypertension, or high blood pressure, could….