Health

With osteoarthritis emerging as the most common cause of immobility among silvers, India leads the way in orthopaedic solutions, writes Srirekha Pillai
Watching a sprightly Usha Bhatia doing the shirshasana (headstand), it is difficult to believe she has implants in both knees. Bhatia underwent bilateral knee replacement surgery—total knee replacement (TKR) in both knees in one sitting—in 2015. “I’m used to an active lifestyle,” says the 71 year-old art connoisseur from Mumbai. “Thankfully, a month after the surgery, I could resume my routine.” Today, she does yoga, household chores and sits cross-legged on the floor while doing puja. “My gait is back to normal now and I don’t have to live with excruciating pain.” Bhatia put up with severe pain for years, trying warm and cold compress alternatively for her joints and wearing a kneecap. “It was only when my gait became crooked that I realised I needed surgical help,” she adds.
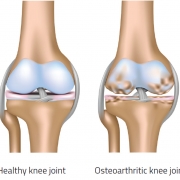
For many silvers like Bhatia, osteoarthritis (OA), a degenerative joint disease where cartilage—ends of the bones that cushion the joints and help support our weight when we walk, run, bend and stretch—deteriorates and disintegrates, causing pain, stiffness, swelling and numbness, is a painful reality. Yet, the majority of the afflicted population, in small towns and villages especially, resists surgery, putting up with severe pain owing to psychological blocks and financial constraints. Take, for instance, 84 year-old Gopalakrishna Panicker from Alleppey in Kerala, who is homebound for two years. Unable to walk without support, his movements are severely restricted. “Why should I go in for a surgery in the autumn of my life?” he asks. There are many like him, reluctant to go under the knife because of advancing years. They compromise on the quality of life, while striking a lifelong companionship with debilitating pain.
UNDERSTANDING OA
OA commonly affects the joints in the knees, hands, feet and spine; the most overworked but neglected parts of our body. Initially, the symptoms, including severe pain and joint inflammation, may only manifest following rigorous activities and exercise, but may become nagging over a period of time, affecting daily activities such as walking, cooking and gardening. Take a short quiz to check whether you are at risk. Silvers are at a higher risk of joint inflammation not just because of OA but age-related wear and tear as well. The physical disability arising from pain and loss of functional capacity owing to joint inflammation can reduce quality of life and increase the risk of further morbidity. OA also takes an emotional toll on the patient and the immediate family.
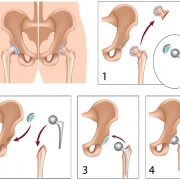
In the initial stages, medicines, physiotherapy and other arthroscopic interventions may work, but in end-stage arthritis, total replacement of the joint—removing the damaged part and inserting a prosthesis or implant—is the only definitive treatment. Among such arthroscopic procedures, the most popular are TKR and total hip replacement (THR).
While OA culminating in joint replacement is usually related to ageing, it is also associated with modifiable risk factors such as obesity and lack of exercise, and non-modifiable risk factors such as genetic predisposition and bone density. Today, OA is seen as the single most common cause of immobility in older adults, with over 10 to 15 per cent of silvers displaying some degree of OA, with its prevalence higher among women.
The World Health Organisation (WHO) estimates that by 2050, people aged over 60 will account for more than 20 per cent of the world’s population. “Of that 20 per cent, a conservative estimate of 15 per cent will have symptomatic OA, and onethird of these will be severely disabled,” a study by the organisation predicts. This implies that by 2050, 130 million people will suffer from OA worldwide, of which 40 million will be left severely crippled by the disease.
INDIAN DILEMMA
A study by Ace Business and Market Research Group (ABMRG) states that in India, most people above 60 suffer from some kind of bone and joint disease and have an immediate need for joint replacement surgery. “A high prevalence of arthritis primarily in north and south India and increasing prevalence of osteoporosis among post-menopausal women in urban areas who follow a sedentary lifestyle have stimulated the growth of the joint replacement market,” the report observes.
Indeed, a rapidly greying population and sedentary lifestyle are contributing to a spurt in OA cases among Indians. “Indians have a genetic predisposition for knee arthritis mainly because of our habit of squatting,” notes Sreedhar Singh, senior orthopaedic surgeon, Columbia Asia, Bengaluru. “The recent rise in prevalence of OA in Indians is primarily because of increased lifespan and a sedentary lifestyle.”
With arthroplasty—the surgical reconstruction or replacement of a joint—gaining ground as the only option for dealing with severe OA, a white paper titled Indian Orthopaedic Devices Market recently published by Sathguru Management Consultants claims that the Indian orthopaedic device market is estimated to grow around 20 per cent a year till 2030.
Noida-based senior orthopaedic surgeon Sushil Sharma, chairman of the Arthritis Foundation of India—an NGO that carries out organised social work in the field of osteoporosis and arthritis—points out that awareness is on the rise, especially in urban areas. “Joints are becoming a priority in the cities,” he says. “People don’t want to stay disabled any longer.” However, the gap between those needing surgeries and opting for it is widening. “According to our estimates, over 500,000 joint replacement surgeries per year are needed to address end-stage arthritis in India. But only about 150,000 surgeries are being carried out every year,” he notes, pointing to a financial crunch as a major handicap in patients opting for replacement surgeries. To make surgical intervention more affordable and root out “unethical profiteering”, the Government recently capped the prices for implants.
MARKET WATCH
That said, with over 150,000 joint replacement surgeries conducted annually, and a 20 per cent increase each year, India is fast emerging as a leading market for joint replacement surgeries. A boom in medical tourism, with the lack of expertise in joint replacement surgeries in Africa and the Middle East, is also a contributory factor in making India a favourite destination for those seeking knee and hip arthroplasty. In the research paper Overview of Orthopaedic Joint Replacement Market in India, Frost & Sullivan concludes that “the market for orthopaedic implants promises to be one of the most lucrative segments in the Indian medical devices market”. The joints market is mostly split between knee and hip procedures. While globally the hip market is larger than the knee market, in India the situation is the reverse, with knee arthroscopy dominating the joint replacement market. Almost 75 per cent of joint replacement surgeries in India comprise knee replacements. Sathguru reports that for every single hip replacement in India, there are at least five knee replacement surgeries. “This is owing to hereditary and lifestyle factors, where the Indian knee sees far more wear and tear than the hip,” it states. “Our knee replacement figures match Western ones,” observes Vinay Joshi, orthopaedic surgeon, Kokilaben Dhirubhai Ambani Hospital, Mumbai. “Fortunately for us, hip arthritis is very low in India.”
The most common reason for total hip replacement continues to be a fall, especially in the silver years. Eighty year-old B B Shettigar from Udupi had to undergo emergency hip replacement following a fall from bed last June. “My parents didn’t realise the severity of the fall as there was only swelling but no pain. They didn’t seek medical help. The next day, my dad couldn’t move an inch because of unbearable pain,” recounts his daughter Shashita. “I still remember the way he was writhing in pain when he was put on a stretcher because the lower part of his body had to be assembled together as the hip joint had cracked.” Now, three months after the surgery, Shettigar ambles in his garden without a walker, climbs the staircase and does simple household chores.
CUTTING-EDGE SOLUTIONS
Today, India is seen as a leader in orthopaedic technologies, surgical solutions, quality prosthetics and equipment, and has emerged as a leading destination for knee and hip replacement procedures. Earlier, not many were willing to undergo surgery because of the risks involved—prolonged recovery period, infections, quality of implants and the risk of implant failure—preferring alternative, non-surgical treatment such as physiotherapy, exercises and yoga.
However, times are changing. Innovations in implants and surgical methods are designed to ensure painless, zero-error procedures, faster recovery—with patients going home the same day or the day after surgery—and longer life of the implant. Allaying fears that knee and hip implants need a revision surgery because of their short lifespan, Singh says, “Earlier, implants lasted only eight to 10 years, necessitating a revision procedure. With advancement in technology, we now have implants that last nearly 20 years. So, if a patient in his 60s goes in for replacement, chances are the implant might last lifelong.”
Incidentally, India became the first country outside America to carry out robotic-assisted TKR recently, when a 67 year-old in Pune, who was bedridden for almost six months owing to a severely deformed knee, was operated upon in July this year.
Narendra Vaidya, managing director and chief joint replacement surgeon, Lokmanya Group of Hospitals, who conducted the surgery, says, “Robotic-assisted TKR is a state-of-the-art technology that enables surgeons to replace the knee joint to half-a-mm precision, which may not be visible to the naked eye. It’s a minimally invasive procedure that rules out cutting the bone, ligaments, etc, thus preserving the natural knee structure.” The procedure, which takes just under 30 minutes, helps the surgeon map the diseased cartilage and prepare a three-dimensional virtual replica of the knee joint on the computer screen on which the prosthesis is virtually placed and aligned before the final execution. Besides bringing in 100 per cent precision in prosthesis placement, robotic-assisted TKR enables better movement, allowing the patient to squat and sit cross-legged, as all the ligaments of the knee are preserved. “Robotic-assisted surgery works best for seniors who display co-morbidities. With the kind of accuracy it brings in, the longevity of the implant is assured,” Vaidya emphasises.
Another case in point is the revolutionary ‘zero technique’—which reduces surgical time for TKR to eight to 10 minutes—propagated by Vikram Shah, the Indore-based winner of the B C Roy International Award 2003 for his work in joint replacement surgery. It is based on the premise that the lesser time a patient spends in the operation theatre, lesser the tissue trauma and faster the recovery. In fact, under this procedure, patients are assisted to walk within four hours of surgery to ensure maximum flexion of muscles.
With hi-tech implants engineered to ensure better mobility, fit and shelf life, the consumer is spoilt for choice today. Brushing aside as a “myth” the perception that imported knee implants are more suited for the Western knee, Joshi says, “Imported knees have a very good track record and have done exceedingly well with our patients.” Physicians prefer to use international products because of their superior technology and proven track record, accounting for nearly 80 per cent of the market. However, one of the widely used indigenous knees is the ‘Indus knee’ developed by Pune-based orthopaedic surgeon K H Sancheti in 2007. At ₹ 32,000-35,000, it’s just one-third the cost of an imported knee. Besides being cost-effective, it allows more than 130-135o of knee-bending, allowing patients to sit cross-legged on the floor.
Talking of indigenous solutions, RMS Regrow by Mumbai-based Regenerative Medical Services is a regenerative cell therapy for knee and hip problems in the early stages of arthritis and joint inflammation. “Our products Chondron and Ossron for cartilage cell therapy and bone cell therapy can be effective in restoring a normal active lifestyle in anybody from 16 to 65 years, eliminating pain completely. We heal joints using the body’s own cells,” says company chief scientific officer and executive director Satyen Sanghavi. “We have had patients who have run marathons after the treatment!” Incidentally, Ossron is the world’s first bone cell therapy product, while Chondron is India’s first cartilage cell therapy product. As part of the treatment, cartilage defects of the joints are treated using the body’s own cartilage cells, which are cultured and multiplied for almost four weeks and then implanted into the damaged joint, helping new cartilage regeneration.
EVOLVING TRENDS
In its analysis of robotic-assisted versus conventional surgical techniques, Frost & Sullivan’s white paper Comprehensive Care for Joint Replacement suggests that those who undergo robotic-assisted surgeries have faster rehabilitation and better long-term outcomes. The paper pegs robotic-assisted arthroplasty as the standard of care in coming years. “Robotic surgery is a step forward in taking precise cuts after computer navigation. It has a bigger role in the precise placement of uni-compartmental—changing half the knee—replacement,” says Avinash Date, consultant arthroplasty and trauma surgeon, Kokilaben Dhirubhai Ambani Hospital, Mumbai. “Computer navigation and patientspecific instruments have further increased the efficiency of the procedure.”
There have been advances in materials as well. Previously, in hip replacements, a metal ball on plastic—ultra-high-density polyethylene—was used. But now with material advances, a ceramic ball in ceramic socket is preferred, as there is much less wear and increased longevity. Another material gaining popularity in hip and knee replacements is oxinium (oxidized zirconium), which has better surface properties and is a tougher material.
IN CONCLUSION
As the No. 1 cause of disability around the world, arthritis can seriously limit mobility, affecting routine activities such as walking, climbing, bathing and other daily tasks. However, awareness about joint replacement surgery is still very low in India. Surveys reveal that only about 10 per cent of people are aware about detection and prevention of joint-related problems such as osteoporosis. It is imperative to raise awareness about the issue among the public.
With the Government still shying away from taking an active role in creating awareness about arthritis and joints, NGOs like AFI, who have created an app specifically to keep a check on bone health have been stepping in to fill the lacunae. “Early diagnosis and treatment of arthritis can avoid joint deterioration,” says Sharma, who is a consultant with Kailash Hospital, Noida. AFI has been regularly holding free health check-up camps across India, where bone mineral densitometry tests are done and medicines distributed. In association with resident welfare associations, they have also been organising ‘Walk with Ease’ camps in various cities such as Delhi, Mumbai, Bengaluru, Dehradun and Jalandhar to educate silvers about the need to constantly monitor their bone health.
In fact, an extensive rehabilitation programme comprising movements and exercises to help the patient adjust to the new joint and begin walking again is just as significant as the early diagnosis and treatment of the joint. It’s important to set proper expectations and avoid high-impact activities such as running and skiing. Moderate use of the implant will increase the odds that it will last longer.
The challenges aside, let’s make no bones about the good news: with advancements in treatment that ensure accurate positioning and longevity of implants and quicker recovery, it’s time to take a break from pain!
ONE-MINUTE RISK TEST
- Is getting up from a seated position or standing for a long time a painful experience?
- Does nagging knee pain disturb your sleep?
- Do you face difficulty while carrying out routine work?
- Has the pain persisted for over three months?
- Do you feel continuous or intermittent stiffness and swelling in the joints?
- Do you avoid climbing stairs because of pain in the joints?
- Did your parent or grandparent suffer from arthritis?
If your answer is ‘yes’ to most questions, you are at risk for osteoarthritis and should go in for a bone density test.
APP-LY ‘MY BONES’
The Arthritis Foundation of India has created a mobile app, ‘My Bones’, to help you diagnose your bone health. You just need to answer 10 questions to ascertain the status of your bones. If the app diagnoses a problem, it gives you advice regarding treatment as well. Further, it gives you dos and don’ts regarding bone health.
GOVERNMENT TAKES NOTE
With the number of knee replacements in the country not reflecting the actual need, the Government recently capped the prices of orthopaedic knee implants. With this, cobalt-chromium implants used in TKR, which is preferred in 80 per cent of knee replacement surgeries, are capped at ₹ 54,720, as against the earlier market price ranging from ₹ 150,000 to ₹ 250,000.
Similarly, TKR implants made of special metals, such as titanium and oxidised zirconium, cannot have a price of more than ₹ 76,600, which is far less than the earlier rates hovering between ₹ 250,000 and ₹ 450,000.
According to the government directive, hospitals should not charge more than ₹ 56,490 for high-flexibility implants that otherwise carried an average MRP of ₹ 181,728.
“POSTPONING SURGERY CAN CAUSE FURTHER COMPLICATIONS”
An interview with Dr Avinash Date, consultant arthroplasty and trauma surgeon, Kokilaben Dhirubhai Ambani Hospital, Mumbai
Who is the ideal candidate for joint replacement surgery?
All replacements or arthroplasties are for pain from arthritis. Pain is partly a subjective feeling. Hence, the severity might vary from person to person. If a person with arthritis is not able to do the things he or she wants to do because of pain in the joint, replacement should be done. For instance, if a person wants to play badminton but is unable to because of pain, he is an ideal candidate for joint replacement.
What should one keep in mind while opting for joint replacement?
People and even doctors have the misconception that you need to postpone joint replacement as much as possible. This is not true. Postponing simply means living with pain longer. This not only wastes your muscles, changes your gait and causes spine problems, but can also in due course lead to health problems such as diabetes, obesity, hypertension and depression, to name a few. The earlier the surgery, the better.
How long does one need to stay in hospital after surgery?
Recovery time may vary from person to person depending on the patient’s health. But, by and large, a hospital stay of five days after the operation is sufficient.
What does post-operative care generally entail?
This differs in hip and knee replacement. All said and done, it is an artificial joint and cannot mimic a normal joint in its behaviour. So avoiding certain movements will prolong the life of a joint.
How soon after the surgery can one start walking or indulge in a maximum range of movements?
If a patient is able to tolerate the pain, he can start walking the same day. But it is better that the patient recovers for a couple of days and then starts standing first and gradually starts walking. To resume normal activities, it takes around six weeks.
Does life go back to normal after surgery or are there restrictions?
Some restrictions will remain after the operation. For instance, after total hip replacement, we ask the patient to avoid flexion and adduction (the movement we make while putting a sock on), which increases the possibility of dislocation. Having said that, there are newer designs that allow you to do that. It’s the same with total knee replacement as well. There are high-flex implants that allow full flexion.
How can one rule out complications such as infections and clots after surgery?
As far as infection is concerned, prevention is better than cure. I always test all my patients for MRSA, which is a dangerous bug that could be harbouring in a patient’s body. If it is present, it needs to be treated first. We also look for other infections such as urinary infection. Our theatres have high efficiency particulate air (HEPA) filters; we use space suits while operating; and use disposable isolation drapes. This theatre discipline reduces the possibility of infection to near zero.
What is the lifespan of an implant?
The life of an implant and failure of an implant are two different things. These days, because of advances in material technology, the possibility of wear has reduced significantly. Failure of the implant is generally because of aseptic loosening, which occurs just underneath the implant because of weakening of the bone.
How does computer-assisted surgery score over traditional surgery?
It has been proven that computer-assisted surgeries reduce the number of outliers as far as the alignment of the prosthesis is considered. But it doesn’t have a direct correlation to the final outcome and patient satisfaction.
Are Indians as an ethnic group more prone to arthritis, especially of the knees?
Incidence of knee arthritis is almost the same in Indian and Western population. But incidence of primary hip arthritis is much more in the West compared to India.
Why do we prefer imported implants?
All the research and development about knee implants has been done in Western countries. That’s why almost all the knee implants are imported, except a few. As far as hip replacement is concerned, Indian implants are as good as imported implants and much cheaper. So, for hips, we use imported as well as Indian implants.
For a patient with deterioration in both knees, is bilateral knee replacement in a single sitting recommended rather than two sittings?
Every surgery leads to a stress response by the body. Two surgeries will lead to a bigger stress response. The heart and other body systems should be fit enough to take the stress of two surgeries. Technically, two surgeries are possible. But for that, the patient needs to be fit enough. Orthopaedic surgeons, with anaesthetists and cardiologists, assess the patient’s fitness for bilateral knee replacement and only then recommend them for surgery. If there is any doubt postoperatively or even intraoperatively, we do only one replacement. There are obvious advantages of bilateral replacement, especially if the deformities are significant. Correction in both knees improves the walk significantly.
Is there an upper age limit for such surgeries?
One needs to consider the physiological age of the patient, not the physical age. If a patient doesn’t have health issues, physical age doesn’t matter.
What are the dos and don’ts after surgery?
It is better to take care of your replaced hips and knees. These are expensive parts. Patients need to take care for them to last long. Avoid doing silly things in enthusiasm, especially within the first year of surgery. Once the pain has gone, people tend to walk more and travel more. Walking fast makes them more prone to injuries, including fractures. It’s also better to avoid sports in the first six months after surgery as patients can be prone to injuries.
Photos: 123RF.com Featured in Harmony — Celebrate Age Magazine October 2017
you may also like to read
-
Hot tea!
If you enjoy sipping on that steaming hot cup of tea, think twice. New research establishes a link between drinking….
-
Weight and watch
If you have stayed away from lifting weights at the gym, thinking it might not be a good idea for….
-
Toothy truth
Research has established a clear association between cognitive function and tooth loss when cognitive function score was categorised into quintiles…..
-
PRODUCT OF THE MONTH
Automatic Blood Pressure Monitor Measure your blood pressure and pulse rate with no fuss Hypertension, or high blood pressure, could….