Health

Obesity is a major health hazard with no one-size-fits-all solution. However, a long-term realistic goal and approach can tip the scales in your favour, writes Srirekha Pillai
How often has your resolution to shed that excess baggage crumbled as fast as the cookie touching your lips? For 67 year-old Saudamini Nayar, who has been on a diet for the past six months, it’s an all too familiar scenario. Weighing 114 kg, she suffers not just from morbid obesity but osteoarthritis and diabetes. Though bedridden for two years and instructed to lose another 24 kg so she can be up on her feet, Nayar cajoles her eight yearold granddaughter to sneak in an extra cookie or piece of cake.
Many silvers like her are struggling to lose weight and keep it off, while coping with ailments that walk in unannounced in the wake of obesity. Indeed, obesity is a global epidemic today, cutting across all ages. In India, it has reached epidemic proportions, with the latest data indicating that over 30 million Indians are obese, a figure that is expected to double in the next five years. With incomes rising and India’s integration in global food markets, the average caloric intake per individual has been on the rise, even as physical activity has been on the decline. In fact, according to the World Health Organisation (WHO), 1.2 billion people worldwide are overweight, making obesity the greatest health threat of the 21st century.
With silvers, too, turning obese, the dangers of an early onset of chronic morbidity and premature mortality are all too real. “Obesity has been on the rise in the past few decades, thanks to a diet rich in sugar and carbohydrates, decrease in physical activity and rise in stress levels,” observes Sachin Jhawar, director of Apex Hospital, Jaipur. “Many silvers are living alone these days, leading to high stress.” As Jhawar points out, chronic stress can lead to increased cortisol levels, stimulating excess glucose production in the body, which gets converted and stored as fat.
Understanding obesity
As defined by WHO, obesity is a chronic disease caused by abnormal or excessive fat accumulation, to the extent that health may be impaired. A body mass index (BMI) ≤30 kg/m2 and weight circumference (WC) greater than 102 cm in men and 88 cm in women is classified as obesity according to WHO guidelines. BMI is calculated by dividing a person’s weight in kilograms (kg) by his or her height in metres squared, while WC is calculated by dividing waist circumference by hip measurement.
Excess fat mass is thought to lead to chronic, low-grade inflammation that is associated with an increased risk of ill health such as metabolic and cardiovascular disease, musculoskeletal problems, decreased physical function, and some types of cancer.
The obesity paradox
Obesity has risen dramatically worldwide over the past few decades. According to “Obesity and Weight Management in the Elderly”, a study published in the British Medical Journal in 2011, sarcopenic obesity—gain in body fat but loss of muscle mass and functional capacity—is common in silvers, further aggravated by the lack of physical activity.
However, it is generally observed that obesity is not as harmful in silvers above the age of 80 as the mortality rate associated with it tends to fall thereafter. The association between BMI and mortality becomes weakened primarily because silvers with low body weight comprise a mix of those who have always been lean and physically active and those who have lost weight through chronic, covert or overt ill health, and cigarette smoking, but are often physically inactive. There is usually some height loss also with ageing, making BMI data even more difficult to interpret in silvers. Further, the reduction in muscle mass—an important determinant of physical function and metabolic rate—leads to the clinical hazards of obesity appearing at a lower BMI in silvers.
Therefore, increasingly, WC is being used as an accurate index of adiposity in adults worldwide. The advantage of WC over BMI is that it correlates highly with both total and intra-abdominal fat. Of late, research has consistently been supporting the notion that abdominal fat distribution and relative loss of fat-free mass is more important than BMI in determining the health risks associated with obesity in silvers.
Facts and figures
The rapid rise in prevalence of obesity across the world has caught health organisations by surprise. According to WHO statistics, 2.8 million adults die each year directly or indirectly as a result of being overweight or obese. According to the WHO report, “Obesity: Preventing and Managing the Global Epidemic”, the prevalence of obesity among adults aged 65 and above increased from about 12 per cent in 1990 to 19 per cent in a decade. The data shows that though the percentage of silvers who meet the recommended level of physical activity—30 minutes of moderate intensity activity for five or more days per week—increased marginally, it is still relatively low, with women having a consistently lower level of recommended activity than men.
Closer home, according to studies, central (abdominal) obesity is a cause for concern among Indians. “Geriatric Health in India: Concern and Solutions”, a report published in the Indian Journal of Community Medicine, argues that silvers belonging to middle and higher income groups are more prone to developing obesity and related complications owing to a sedentary lifestyle following retirement. Co-morbidities and medications (several of which tend to cause obesity) are other contributory factors.
Women vs. Men
New research shows that women are more likely to be obese than their male counterparts. A study published in British medical journal The Lancet put the number of obese women in India in 2014 at 20 million, compared to 9.8 million obese men. According to the National Family Health Survey conducted in 2015-2016, one-fifth of Indian women are obese.
Local surveys seem to corroborate this. A 2005 survey among those over 65 years in Chandigarh pegged obesity among women at 42.1 per cent, compared to 20.9 per cent among men. In another study conducted among 206 silvers attending the geriatric clinic at a tertiary care hospital in Delhi, women again beat men in obesity with the former comprising 40.3 per cent compared to 34 per cent among men. Similarly, a study conducted in Kollam district of Kerala in 2014 among those over the age of 60 also revealed a larger percentage of obesity among women—49 per cent—compared to 35 per cent in men.
This, experts say, could be because of psychological factors and weight gain during pregnancy.
Health risks
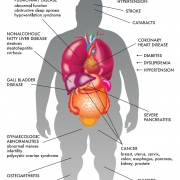
Several studies have linked obesity in silvers with difficulty in performing physical functions and daily tasks such as walking, climbing stairs, rising from the chair or bed, picking up an object from the floor and lifting heavy objects, among others. “Obesity can lead to not just other health issues like diabetes and heart disease, but also cause mechanical issues such as knee pain, wear and tear of the joints, varicose veins and arthritic issues, affecting mobility,” points out Dheeraj Kapoor, endocrinologist at Kokilaben Dhirubhai Ambani Hospital, Mumbai. “The super obese can also suffer from sleep apnoea, where the body doesn’t get enough oxygen.”
SOME HEALTH HAZARDS THAT ACCOMPANY OBESITY ARE:
Type 2 diabetes: The single best predictor of type 2 diabetes is being overweight or obesity. Almost 90 per cent of people living with type 2 diabetes are overweight or obese. People who are obese have added pressure on their body’s ability to use insulin to properly control blood sugar levels, and are therefore more likely to develop diabetes.
Cardiovascular diseases: Obesity, especially abdominal obesity, is a very important risk factor for cardiovascular diseases. India accounts for about 60 per cent of the world’s heart disease burden, despite having less than 20 per cent of the world’s population. NGOs such as the Indian Heart Association (IHA) have been raising aware ness about this issue. Sishir Rao, resident physician in diagnostic and interventional radiology at the Massachusetts General Hospital and a clinical fellow at Harvard Medical School, and co-founder of IHA, along with Sevith Rao, medical student at Baylor College of Medicine, Houston, points out, “There are numerous functional implications of obesity in silver years, including the rising incidence of cardiovascular disease, diabetes, metabolic syndrome, and arthritis. These problems are often compounded by the decrease in physical activity and energy expenditure as individuals get older.”
Hypertension/stroke: As recently outlined by the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research, advanced years and obesity are two of the most powerful risk factors for uncontrolled hypertension, which in turn is a major determinant of mortality and stroke.
Arthritis: Obesity and arthritis go hand in hand. Sustained period of excessive strain in silvers can end up in osteoarthritis of weight-bearing joints. It’s a vicious cycle, wherein patients with severe arthritis who are unable to perform physical activities end up gaining more weight.
Alzheimer’s: Studies also indicate a connection between obesity and reduced brain volume, linking it to vascular dementia and Alzheimer’s. The Framingham Heart Study comprising male participants aged 55 to 88 years detected a link between obesity and dementia. It found that the risk for Alzheimer’s increased by 36 per cent for every BMI unit at the age of 70 years and above.
Respiratory disorders: Weight gain is associated with a decrease in lung volumes and shortness of breath. Obesity is also responsible for obstructive sleep apnoea, caused by a blockage of the airway. Excessive adipose tissue on the neck, thorax and abdomen results in a number of pulmonary function abnormalities, leading to complications such as obesity hypoventilation syndrome, a condition in which a person fails to breathe rapidly or deep enough, resulting in low blood oxygen levels and high blood carbon dioxide levels. Asthma is also more common in the obese.
Cancers: Obesity increases the risk for many forms of cancer as well. Over 7 to 15 per cent of breast cancer cases and 11 to 14 per cent of bowel cancer cases are attributed to obesity. Studies have indicated that post-menopausal women with a BMI of over 28 kg/m2 have a 26-per cent increase in risk of breast cancer. Higher oestrogen levels in obese post-menopausal women compared to their leaner counterparts are thought to promote carcinogenesis. The American Cancer Society’s Cancer Prevention Study has shown a risk of colon cancer greater by 75 per cent in men and 25 per cent in women with a BMI of 30 kg/m2. Obese post-menopausal women are also at a high risk of malignant melanoma and endometrial cancer, while silvers who are obese are at an increased risk of other forms of cancer such as gallbladder, pancreatic, renal, uterine, cervical and prostate cancers.
Urinary incontinence: Strain, stretch and eventual weakening of neuromuscular structures, along with the apparent excessive weight and pressure applied on the bladder by increased intra-abdominal fat mass, can result in incontinence. Diabetic patients are at a higher risk of incontinence.
Sexual dysfunction: Studies link central obesity with erectile dysfunction in men over the age of 60. Though age appears to be a major determinant of erectile dysfunction, obesity increases the chances for impotence. In a cross-sectional analysis of men over 50 in the US Health Professionals’ study, obesity, independent of other confounding factors, increased the risk of erectile dysfunction by 30 per cent.
Non-invasive solutions
In silvers, the aim of weight loss is to improve physical function and quality of life with emphasis on cardiovascular risks. Even moderate weight loss may bring about dramatic improvement in mood and mobility. “There are no quick-fix solutions to weight loss,” says nutritionist and obesity consultant Naini Setalvad. “Following fads or skipping meals won’t help. A balanced diet consisting of proteins, fats and carbohydrates along with moderate exercise will yield results.” Her own inspirational life story (‘From 160 kg to 60 kg’) is testament to the ancient wisdom of eating right and in moderation. In her column for Harmony-Celebrate Age, ‘Nutritalk’, she shares some simple tips to keep weight gain at bay (‘Fight fat with food).
An ideal diet plan is customised depending on the age, weight and medical history of the patient (‘A healthy balanced diet will do the trick’). However, there are a few food items that can be ticked off for good from our plates (Skip them). A combination of exercise and modest calorie restriction appears to be the optimal method of reducing fat mass and preserving muscle mass to combat sarcopenic obesity, most commonly associated with health risks in silvers. “The safest way for silvers to lose weight is like anybody else: Go on a diet, have your meals on time, get proper sleep and exercise for at least 30-40 minutes daily or at least five to six days a week,” says Kapoor. “Simple aerobic exercises and walking will go a long way in combating obesity.”
As polypharmacy (the use of multiple medications) is common among silvers, the benefits and risks of anti-obesity drugs should be considered while introducing them. There is an urgent need to adopt a multidisciplinary approach to weight control through awareness campaigns and strategies to increase physical activity and change eating behaviour. A preventive health package should include weight management, good nutrition, balanced diet and physical exercise. Proposing a well-rounded model, the Rao brothers say, “We at the Indian Heart Association believe any therapeutic plan should incorporate weight loss strategies, physical activity, healthy diet, and careful follow-up with medical professionals.”
Any weight loss programme should be tailored according to individual needs, keeping in mind the age, along with other vital parameters and depen dency on drugs. Weight loss should be routinely monitored, as most silvers are on drugs, and even moderate weight loss could fluctuate vital parameters, altering the need for certain drugs such as diuretics, hypoglycaemics and analgesics.
The surgical option
Bariatric surgery has been mired in controversy, especially regarding its effectiveness and safety for silvers. There is also a lot of confusion regarding the upper age limit for such a surgery (’70 is the cut-off age for surgery’). However, recent studies point out that silvers should not be denied the opportunity to go under the knife for losing weight based solely on their age. Though there is a paucity of studies on silvers operated upon in India, data from 150 patients—cutting across all ages—operated in Delhi between 2006 and 2009 shows that surgery helped in controlling diabetes in 88.4 per cent, hypertension in 58 per cent, and increased heart-protecting good cholesterol (HDL) in 93 per cent and triglycerides in 82.1 per cent.
International studies that are silver-specific seem to affirm the benefits of the surgery. And the position paper by the European Society for the Study of Obesity outlines that selected elderly people should also be considered for surgery, eliminating the upper age limit. “The overall primary surgical goal should be to slow the functional decline trajectory,” it argues. Following the surgery, silvers, like younger patients, may see improvements in medical conditions related to obesity such as diabetes, hypertension, arthritic pain, etc.
Jhawar quotes the instance of a 55 year-old lady from Jaipur who was morbidly obese at 140 kg and immobile. “When she came to us, she was highly diabetic, and was on 100 units of insulin per day. A year since surgery, she’s 30 kg lighter and able to walk around. With her diabetes in the manageable range, she’s on oral medication now.”
In conclusion
According to a 2011 study, the life expectancy of Indians in the past 50 years has been increasing exponentially, thanks to better medical facilities. With obesity on the rise among a rapidly ageing population, it’s time for a proactive approach. Policymakers should focus on well-rounded antiobesity measures and awareness campaigns.
Here’s the silver lining though: a WHO report that lists obesity as one of the 10 most preventable risk factors affecting the global population. The ball, evidently, is in your court—game on!
FIND YOUR BMI
- BMI is used in determining obesity.
- It is a number calculated by dividing a person’s weight in kilograms by his or her height in metres squared. An adult with a BMI of 30 or greater is clinically obese.
- Though it’s not an actual percentage of body fat, it is a good indicator to categorise weight in terms of what is healthy and unhealthy.
- You can check your BMI online at https://obesityfoundationindia.com/bmi.htm
SKIP THEM
- Fried & processed foods
- Aerated drinks
- Fruit juices
- Sherbet
- White flour
- Chocolates & sweets
SHED THE EXCESS BAGGAGE
Obesity treatment strategies vary from person to person. Beginning treatment early is an essential part of success. It’s important to talk to your physician before beginning any weight loss programme. There are several methods for treating obesity such as behaviour modification, physical activity, medically managed weight loss and surgical treatment.
Behaviour modification: Modifying behaviours that have contributed to developing obesity is one way to treat the disease either alone or in conjunction with other treatment. A few suggested behaviour modifiers include changing eating habits, increasing physical activity, engaging in a support group and setting realistic weight management goals.
Physical activity: Increasing or initiating a physical activity programme is an important aspect in managing obesity. Set realistic goals and make sure to consult your doctor before initiating any exercise programme.
Medically managed weight loss: Medically managed weight loss programmes provide treatment in a clinical setting with a licensed healthcare professional, such as a medical doctor, registered dietician and/or psychologist. These programmes typically offer services such as prescription of weight loss medications, nutrition education, physical activity instruction and behavioural therapy.
Surgical treatment: Surgical treatment of obesity is an option for those who are classified as morbidly obese. Morbid obesity is defined as a patient with a BMI of 40 or greater, or weighing more than 40 kg over their ideal body weight. In addition, a patient with a BMI of 35 or greater with one or more obesity-related diseases is also classified as morbidly obese.
Courtesy: Obesity Foundation India
FROM 160 KG TO 60 KG
Obesity, lifestyle and disease consultant Naini Setalvad’s epic transformation from 160 kg to 60 kg was not without hiccups. Her weight yo-yoed with frequent crash and fad diets. Finally, she triumphed. Her journey in her words …
I was born tiny, weighing just 2.7 kg. As I was very active and a small eater, my family worried for me. To make me put on adequate amount of weight, excess sugar and fat were added to my food. Looking back, I realise that my weight gain story started there.
By the time I was in Class 7, I had made the transition from skinny to fat. I had become addicted to unhealthy eating. Now, my family started making rounds of dieticians, worried about my weight. Every year, a new attempt would be made. From hospitalisation to popping pills, slimming powders to meal replacements, high protein diets to starvation and gyms, I was put through everything. But the pattern was similar: I would lose 10 kg and put 20 back on.
At 14 years of age, I weighed 60 kg, and at 18, I touched 90 kg. By 27, I was 149, and by 32, an impossible 160 kg. I could not fit into normal chairs, my body ached, and moving was impossible. I felt like a prisoner in my own body. I resolved that enough was enough. I then embarked on my final weight loss journey. It was simply about the right food combinations, eating seasonal and local vegetables and fruits and moderate cardio exercises. In three years, I lost 100 kg. Today, 18 years later, I have been able to maintain my weight by simply following the above.
OPERATION SUCCESSFUL
The surgical treatment of obesity in silvers remains controversial, largely owing to a lack of data demonstrating its long-term benefits for them. Recent reports, however, imply that there is no significant increase in the risks associated with the surgery for silvers.
A study conducted at Columbia University’s Centre for Obesity Surgery found that patients over the age of 60 who have bariatric surgery enjoy the same benefits as younger people. They also found that post-operative complications for silvers are no more than those for younger people. The study also mentioned that the mortality rate among silvers was about the same as it was for silvers who had heart bypass or hip replacement surgeries.
Another report published in WebMD, an online medical portal, based on a survey of more than 48,000 patients over 65 years who had open or laparoscopic bariatric surgery procedures in US, states that age does not increase the associated risks. To quote study researcher Robert B Dorman of the University of Minnesota Medical School, “If patients are over the age of 65, and otherwise relatively healthy, I think this study gives surgeons an opportunity to tell them that they can undergo these operations with relatively similar outcomes compared to younger age populations.”
According to the report, compared to middle-aged adults, silvers did not appear to be at any increased risk of death or having major adverse events such as heart attacks, strokes, and serious infections after the procedure.
“70 IS THE CUT-OFF AGE FOR SURGERY”
Jaydeep H Palep is consultant robotic, laparoscopic bariatric & GI surgeon, Department of Bariatric Surgery, Kokilaben Dhirubhai Ambani Hospital (KDAH)
With underlying health issues such as hypertension and diabetes associated with ageing and obesity, is it safe enough for silvers to go under the knife?
Yes, obesity surgery is done under strict guidelines laid down by the Obesity Surgery Society of India (OSSI). As per these guidelines, it can be safely offered to individuals up to the age of 70 and sometimes even up to 75 years depending on the merit of the case.
Is there an upper age limit for bariatric surgery?
As per the guidelines, currently 70 years is the cut-off age above which we tend to avoid offering surgery unless left with no other alternative.
Who is the ideal candidate?
Anyone who is of a BMI >37 kg/m2 is straightaway a candidate for weight loss surgery. And any individual who is less than a BMI >37 kg/m2 but more than a BMI of 32 kg/ m2, with at least one medical illness other than obesity, such as type 2 diabetes, hypertension, obstructive sleep apnoea and osteoarthritis, among others, qualifies for surgery.
What are the preoperative guidelines?
A strict preoperative workup is required for any patient undergoing this form of surgery and is inclusive of a preoperative liquid diet and chest physiotherapy. This is especially enforced for all those above the BMI of 40 kg/m2 because the liver in these individuals is enlarged and fatty and it needs to be treated medically prior to the surgery.
Do silvers require a longer hospital stay after the surgery? What are the necessary precautions during this period?
We usually see silvers recover in four days after surgery, going home on the fifth day. It is very important to make sure that these patients are mobilised out of bed early after the surgery. At our institute, we start mobilisation six hours post surgery and continue until the day of discharge. A very special precaution is taken to prevent deep vein thrombosis (DVT)—blood clots forming in the veins of the leg leading to pulmonary embolism, cardiac complications, stroke, etc—by applying pneumatic stockings to patients prior to surgery and continuing until discharge and a single shot of subcutaneous (like an insulin injection) low molecular weight Heparin daily for 28 days.
How many silvers seek surgical help in a month?
We get at least 12-15 patients every month who are above 50 years of age. The numbers have been increasing over the past five years at our institute.
Can you share some interesting case studies?
Recently, we operated on a 58 year-old lady for morbid obesity. She had a BMI of 45 kg/m2, and was confined to a wheel chair for almost two years with end-stage liver disease owing to a non-alcoholic fatty liver. It was a unique case, as it was for the first time in the world that a patient had a living donor liver transplant along with a bariatric surgery done in the same sitting. It has been nine months and she is doing absolutely fine. She comes walking to our hospital for routine follow-up visits.
Another interesting case was that of a 65 year-old morbidly obese lady from Uganda, who came to our hospital on a stretcher for a multi-level disc prolapse and was first offered a spine stabilisation surgery. We did a bariatric surgery on her five days after that. She recovered wonderfully after vigorous physiotherapy and we were able to send her back home in just two weeks. She went back walking!
It is generally believed that the risks of bariatric surgery far outweigh the benefits for silvers. This is pure myth. The risks for any major surgery will only outweigh its benefits if the patient has a very complex and irreparable cardiac or respiratory illness owing to which putting the patient under general anaesthesia is a risk to life. Once such a condition is ruled out in our preoperative assessment and workup, the benefits of surgery will always outweigh any risk whatsoever.
What is the approximate cost of bariatric surgery?
We usually have fixed packages for bariatric surgery at KDAH, ranging from ₹ 320,000 to ₹ 700,000 depending on a variety of factors.
“A HEALTHY BALANCED DIET WILL DO THE TRICK”
Bhakti Samant is chief dietician, Nutrition Therapy Department, Kokilaben Dhirubhai Ambani Hospital (KDAH)
What are the things to keep in mind while putting silvers on a diet?
The factors that need to be considered before planning diets for silvers are:
- Any metabolic disease such as diabetes mellitus, coronary artery disease, renal disease, liver disease, etc
- Dietary recall to be taken to rule out nutritional deficiencies
- Gastro-intestinal disturbance
- Physical activity level [whether they are mobile, need partial support or are bedridden].
Should the diet be customised keeping in mind health issues, age and weight?
Yes, each diet plan is customised depending on the age, weight and medical history. For instance, for a geriatric patient with diabetes mellitus, the diet plan would focus on whole grains and cereals containing complex carbohydrates, and restricting simple sugars while ensuring adequate amount of fibre and protein that are easy to digest.
In patients where movement is restricted owing to obesity and strain on the knees, how far will diet play a role in helping them recover?
Diet would definitely help to reduce the weight in such patients by 5-10 per cent. This weight loss would help them to relieve the symptoms to some extent. It will also help to reduce the progression of the disease. For instance, a 64 year-old woman suffering from morbid obesity and osteoarthritis in both knees was referred to us. She was bedridden. We put her on a low calorie diet with moderate increase in protein and fibre to help her lose weight. She lost almost 10 per cent of her weight, enabling her to move around in the house and independently take care of the household work.
What would be the ideal diet for such patients?
There is no such thing like an ideal diet. A healthy balanced diet that includes all the food groups in the right proportion will do the trick. Whole grain cereals, whole pulses, dal, low-fat milk and milk products, small quantities of nuts, three to four servings of vegetables, two servings of fruits and good levels of hydration should help.
Photos: 123RF.com Featured in Harmony — Celebrate Age Magazine April 2017
you may also like to read
-
Hot tea!
If you enjoy sipping on that steaming hot cup of tea, think twice. New research establishes a link between drinking….
-
Weight and watch
If you have stayed away from lifting weights at the gym, thinking it might not be a good idea for….
-
Toothy truth
Research has established a clear association between cognitive function and tooth loss when cognitive function score was categorised into quintiles…..
-
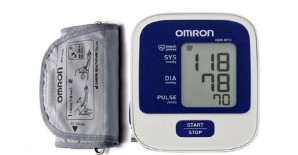
PRODUCT OF THE MONTH
Automatic Blood Pressure Monitor Measure your blood pressure and pulse rate with no fuss Hypertension, or high blood pressure, could….