Health

Postmenopausal bleeding may not be cause for panic but requires prompt attention, writes Shivani Arora.
For women in their 50s and 60s, sudden spotting or bleeding after menopause is cause for concern. To ensure there is no major underlying reason for the sudden bleed, seeking a doctor’s help at the right time is vital. Dr Gita Arjun, director, E V Kalyani Medical Foundation in Chennai, answers our queries on postmenopausal bleeding.
What are the common causes for bleeding after menopause?
Postmenopausal bleeding can be either from the vagina, the cervix (the mouth of the uterus), or from inside the uterus itself. After menopause, the lack of oestrogen causes the vaginal lining to become thin and fragile. Sometimes, this can lead to spontaneous bleeding from the vagina. This can happen some years after menopause. Bleeding from the cervix can be either owing to a malignancy or a benign polyp; the bleeding will stop as soon as the polyp is removed. If malignancy is suspected, a biopsy will be done. Bleeding from inside the uterus could commonly be owing to an endometrial polyp, which is a small benign growth on the lining of the uterus, or a small fibroid in the cavity of the uterus. However, cancer needs to be ruled out.
Generally, is bleeding after menopause a cause for concern?
No. Sometimes the bleed could just mean an occurence of unexpected ovulation, but investigation is needed to ensure there is no other underlying health issue, especially cancer.
The good news is that 90 per cent of postmenopausal bleeding is owing to non-cancerous or benign conditions and only 10 per cent is owing to a malignancy.
What will the doctor do?
The doctor will initially question you on your medications because blood-thinning agents like aspirin could cause bleeding or spotting. Even hormones like oestrogen can cause unusual bleeding. The doctor will then inspect the external genitalia to make sure there is no reason for bleeding, after which the vagina and the cervix are inspected. The doctor will also examine the shape and size of the uterus. If there is no obvious reason for bleeding, you will need an ultrasound, which is the most important test to determine the cause of bleeding.
The ultrasound can help rule out cancer. An internal (vaginal) ultrasound is done to evaluate the thickness of the uterine lining. In postmenopausal women, if the lining of the uterus is less than 5 mm in thickness, it will rule out cancer in 99 per cent of women. The initial risk of cancer comes down from 10 per cent to 1 per cent if the endometrial lining is thin. If the lining is more than 5 mm, the doctor has to determine if the thickening is benign or malignant. This is done through a minor surgical procedure called hysteroscopy in which a thin, lighted tube called a hysteroscope is inserted into the uterine cavity to look for any abnormalities. If there is a small polyp or fibroid, it will be removed. This will usually take care of the bleeding. However, if there is any suspicious or abnormal growth of tissue, it will be sent for testing to rule out or confirm cancer.
Why does cancer happen in the lining of the uterus?
After menopause, sometimes oestrogen is produced abnormally in the body owing to excess body fat which converts other hormones into oestrogen. The oestrogen keeps acting on the lining of the uterus and makes it proliferate. This proliferation is called hyperplasia, which can later form atypical cells. Around 10 per cent of atypical hyperplasias can turn into cancer.
Is a hysterectomy always the answer to deal with the problem?
Postmenopausal bleeding by itself is not a reason to undergo a hysterectomy. You need a hysterectomy only when it has been proven by hysteroscopy that there are atypical or malignant cells.
How can we reduce the risk of postmenopausal bleeding?
Polyps and fibroids cannot be prevented or avoided. However, reducing excess body fat by following a healthy diet and exercise regimen can reduce the risk of producing oestrogen after menopause. If you are undergoing menopause or have already attained menopause, make sure you get fit, have a well-balanced diet, and exercise well to ensure a healthy future.
POSTMENOPAUSAL BLEEDING
When a woman stops having menstrual periods for a year, she is considered to have attained menopause
- 50 Most Indian women experience menopause around the age of 50
- 5-10% of women can develop bleeding after menopause
- 12 months The chances of developing bleeding are highest in the first 12 months after menopause; there are lesser chances as the years go by
- Bleeding can be from the vagina, cervix or the uterine lining
- 90% of bleeding is owing to non-cancerous (benign) causes
Photo: iStock Featured in Harmony — Celebrate Age Magazine March 2016
you may also like to read
-
Hot tea!
If you enjoy sipping on that steaming hot cup of tea, think twice. New research establishes a link between drinking….
-
Weight and watch
If you have stayed away from lifting weights at the gym, thinking it might not be a good idea for….
-
Toothy truth
Research has established a clear association between cognitive function and tooth loss when cognitive function score was categorised into quintiles…..
-
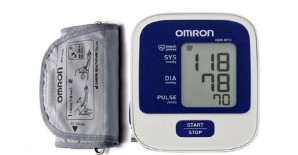
PRODUCT OF THE MONTH
Automatic Blood Pressure Monitor Measure your blood pressure and pulse rate with no fuss Hypertension, or high blood pressure, could….